Take Control of These 5 Common Inflammation Triggers
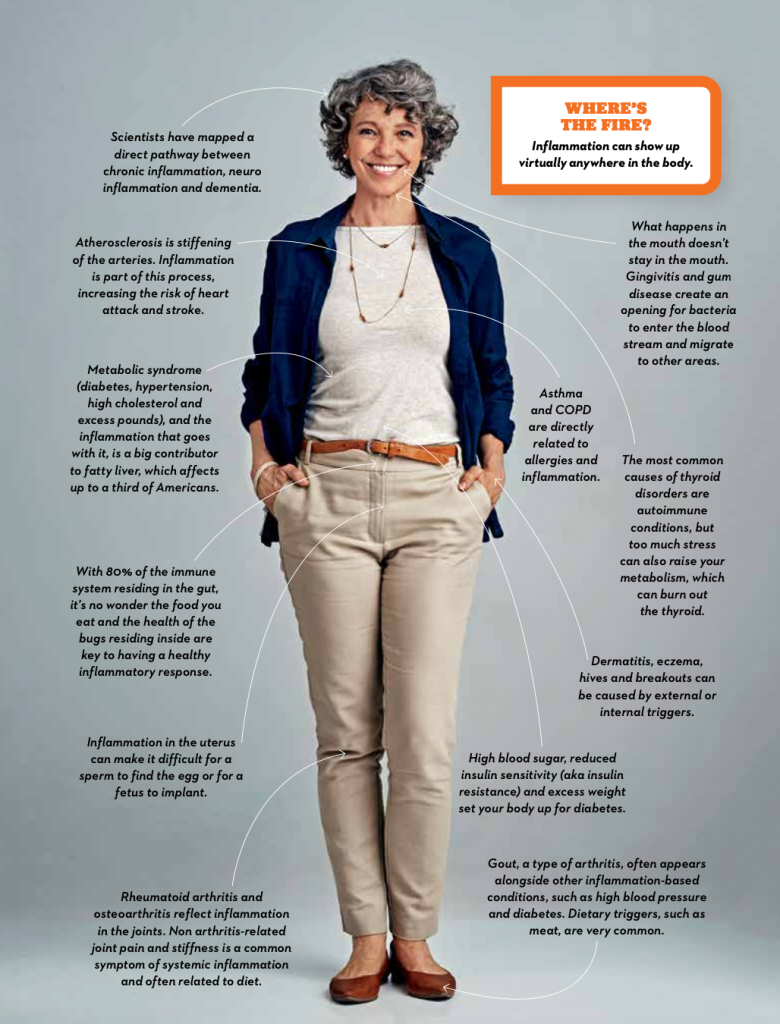
When your immune system is firing blindly at everything around it, it can impact your entire body.

Your body was smartly designed to be a fortress. Thanks to an immune system that is programmed to keep out bad things — even bugs that weren’t in existence when you were born — you don’t have to worry about every odd virus, parasite, or bacterium you might encounter. Besides having built-in barriers in what would otherwise appear to be the most delicate tissues (skin and the mucosa lining your nose, throat, mouth, and the rest of your gastrointestinal tract), your body counters invaders through the process of inflammation. It’s a sign that something is amiss.
If you’ve had allergies, a cold, or even sprained your wrist, you’ve seen inflammation at work. When you have an injury, the immune system releases messenger compounds that bring white blood cells and chemicals to the area to try to protect it. (The swelling and pain are there partially to help keep the area immobile so you don’t continue to injure it.) When a cold virus triggers the invisible tripwire via the nose, mouth, or eyes, your body increases its temperature as a subtle signal to neutralize the virus and releases compounds that work to engulf the virus and shuttle it out of the body — a “no solicitors allowed” policy.
The Right Balance
Just like your nervous system, which functions well when there’s a balance between the sympathetic and parasympathetic arms, there’s a tipping point for inflammation. When the immune surveillance system is turned up too high, your body gets a little trigger happy. It then releases too many of these various compounds, which can damage healthy tissue. Too low and you’re constantly sick.
It’s this too high or ongoing inflammation that contributes to a variety of conditions. This includes heart disease, cancer, diabetes, autoimmune disorders, and more. Those vague, annoying symptoms, such as weight gain, headaches, gastrointestinal complaints, joint pain, and fatigue can be signs that inflammation is getting out of control. Unfortunately, it’s not that easy to track down the source.
“There are many different pathways,” explains Jenny Bennett, ND, a naturopathic doctor and acupuncturist and founder of Aria Integrative Medicine in Seattle. “The immune system’s goal is to fight off foreign invaders. It could be external things such as mold, pollen, anything we eat or ingest, alcohol, or certain types of bacteria that we might touch. But then there are a lot of internal factors that can play a role in immune system function, such as certain types of inflammatory states that are promoted by different types of hormones.” A common example: The balance of the hormones estrogen and progesterone, which fluctuate in perimenopause. “Increases in progesterone and decreases in estrogen might lead to allergies, while increases in estrogen and decreases in progesterone can lead to an autoimmune inflammatory state,” she explains.
From Culprit to Cure
“A lot of people think inflammation is a one-to-one action,” says Sunil Pai, MD, an integrative medicine physician, author of An Inflammation Nation, and founder of the Sanjevani Integrative Medicine Health & Lifestyle Center in Albuquerque, New Mexico (he works with patients all over the US). “If someone has pain and they take an NSAID [non-steroidal anti-inflammatory drug], that’s blocking one pathway. But what we understand is that inflammation is a case of hundreds of signals. It’s the balance between the immune system, epigenetics, the microbiome, diet — these things all trigger this cascade. It’s vast.” Following are the most common triggers for inflammation, whether acute or chronic. Luckily, many of them are within your power to control.
1. SAD Food
That would be the standard American diet, which is high in saturated fat, sugar, and ultra-processed and refined foods, and low in fiber and antioxidant-rich fruits and vegetables. “The SAD is the largest contributor to inflammation,” says Pai. This unhealthy diet, combined with way too little exercise, also allows extra pounds to creep on. Fat, as you’ll learn, is like a factory churning out inflammation. Switching to a plant-based eating style that emphasizes clean, whole, nutrient-dense foods is by far the No. 1 most powerful thing you can do to feel better and turn off inflammation.
2. Elevated Stress
The interactions between stress, cortisol, and inflammation are complicated — due to all
the different pathways we just covered — but suffice it to say that stress is a flamethrower on your entire system. Some cortisol can temper the flames, while too much or too little can fan them. What’s more, high levels of inflammation can also prompt the release of more cortisol, a vicious circle. Learning techniques to reduce stress and change how your body views and responds to it can help regulate the immune system and make it strong without being overly responsive.
3. Poor Sleep
It’s common to have the occasional night spent tossing and turning. However, night after night of restless slumber — or simply ignoring your body’s cues to sleep — leads to chronic inflammation. And it’s not just getting too little sleep. Inconsistent sleep from night to night is also problematic. What’s worse, like stress and weight gain, the relationship between sleep and inflammation is bidirectional.
In a 2020 study, published in Frontiers in Neurology, the study authors concluded that: “… the circadian clock is present in the majority of the body’s cells and corresponds to a 24 [hour] cycle, and inconsistent sleep may promote greater inflammation overall by continual disruption and resetting of these underlying cellular mechanisms.” So the cells are struggling to adapt to the changes, which stresses them, prompting them to churn out inflammatory compounds. Good sleep hygiene, combined with exercise, a healthy diet, and stress management will all work in concert to make it easier to fall and stay asleep.
4. Gut Imbalance
The aforementioned SAD — in addition to stress, lifestyle, aging, illnesses, and drugs — can create an environment in the gastrointestinal (GI) tract that makes it easy for bad bacteria to take hold. These bugs create harmful compounds that circulate in the body (and the healthy compounds created by good bugs are simultaneously reduced). In addition, that imbalance makes the gut lining more permeable, enabling food to get into areas of the gut where it shouldn’t be, triggering the immune system to launch an attack, says Pai. Healthy diet changes that include eating more fiber-rich foods, plenty of plant polyphenols, as well as probiotics — good gut bugs to help repopulate your current intestinal communities — will help keep a check on bad bacteria and heal the gut.
5. Too Many Pills
The drugs you take to counter inflammation — whether it’s antibiotics or over-the-counter pain medications and stomach acid reducers — are contributing to an imbalance of bacteria in the gut that tips the scale toward creating more inflammation. All your healthy lifestyle changes will reduce inflammation so you get sick less often and need fewer meds for pain, reflux, or infections. Have you noticed a theme yet? It’s all about lifestyle, which means you’re in the driver’s seat.
How Strong Should Your Immune System Be?
Stronger isn’t necessarily better when it comes to your body’s ability to attack invaders. A measured response is beneficial, but one that’s too revved up may trigger allergies, which are the sign of an overactive immune reaction. Plus, that too-sensitive system really just goes back to inflammation, says Sunil Pai, MD.
“Conventional medicine says autoimmune problems are your body attacking itself,” he
explains. “But the cell is not designed to attack itself. It’s designed to defend and repair itself.
So there’s a trigger, a bully, that continues to knock the cell. If it can’t repair itself, the cell gives
up and the body turns on itself. [A good doctor will] investigate those triggers and teach you how to restore, rebalance, and rejuvenate your system.” Balancing the immune system involves adjusting your diet, supplements, exercise, and other lifestyle habits so it responds appropriately to “other” [not the body] triggers and then goes back to surveillance mode.
A version of this article appeared in our partner magazine The Complete Guide to Anti-Inflammation.












