The Subtle and Telltale Signs You Have a Pelvic Floor Problem (and How to Treat It)
The disorder is common, but not normal — and you don't have to live with it.

Did you know that one in three women experiences a pelvic floor disorder in her lifetime?
It’s true — a third of women suffer from urinary incontinence, problems passing stool, or pelvic organ prolapse (the three main types of pelvic floor disorders). Urinary incontinence, which affects one in four women, becomes more likely with age; up to 75 percent of women over 65 report bladder leaks. (And pregnancy isn’t the only cause. A 2016 study found that urine leakage is common in women who have not given birth.) Just because pelvic floor problems are common, however, does not mean they’re normal or that you have to put up with them.
“Most women don’t receive timely treatment for pelvic floor disorders due to a lack of awareness, stigma, and inadequate access to pelvic floor physical therapists,” explain Tamara Grisales, urogynecologist and Bijal Toprani, physical therapist. “On average, most women go more than six years before receiving care for certain conditions.”
Not sure whether you have an issue? Dr. Grisales and Dr. Toprani have listed the sneaky signs and telltale symptoms of a pelvic floor problem below. “It’s easy to ignore or miss the warning signs if no one has told you what to look for,” Dr. Toprani adds. “But there are many effective treatments to put an end to these concerns.”
Meet our experts
Tamara Grisales, MD, is a urogynecologist and associate clinical professor at the University of California, Los Angeles. Dr. Bijal Toprani, DPT, is a physical therapist and owner of Liria Physical Therapy and Wellness. Both Dr. Grisales and Dr. Toprani work as experts in pelvic floor disorders at Hinge Health.
What is a pelvic floor disorder?
To answer this, we must first gain a better understanding of the pelvic floor. “Your pelvic floor is made up of the muscles, ligaments, nerves, and tissue that create a natural hammock slung across the pelvis,” Dr. Grisales says. “Pelvic floor disorders (PFDs) include anything that impacts the normal function of your pelvic floor.”
The three main types of PFDs are urinary incontinence, fecal incontinence, and pelvic organ prolapse, when an organ such as the uterus, bladder, or lower intestine herniates or bulges into the vaginal canal, often because the pelvic floor muscles are weak. PFDs can also be caused by hypertonic pelvic floor muscles — when the muscles spasm or can’t relax.
What are the sneaky signs you have an issue?
Here are a few subtle signs of a PFD:
- Pain during sex.
- Pain during gynecological exams (when your gynecologist uses a speculum, for example).
- Low back or hip pain that’s unexplained by musculoskeletal (bones, cartilage, ligaments, tendons, and connective tissue) issues or injury.
Keep in mind that many other conditions cause pain during sex or pain in the low back and hip, including: infection, fibroids, endometriosis, irritable bowel syndrome, and pelvic inflammatory disease. But if you know that your pain isn’t caused by any of these conditions, it can’t hurt to ask your doctor about PFDs.
What are the telltale symptoms of a pelvic floor problem?
While some signs of a pelvic floor disorder are subtle, others are obvious. Dr. Grisales and Dr. Toprani suggest visiting a pelvic floor specialist or physical therapist if you’re experiencing one or more of the following:
- Leaking urine occasionally, constantly, or with certain activities (like coughing, sneezing, laughing, or exercising).
- Urinary urgency and frequency, or feeling like you’ve “gotta go” all the time.
- Difficulty starting to pee or completely emptying your bladder.
- Difficulty passing stool, including frequent constipation, problems with hemorrhoids, fissures, trouble finishing a bowel movement, or leaking feces (staining your underwear).
- Pelvic pressure, bulging, or a feeling of heaviness in your vagina.
- Weak, separated, or postsurgical abdominal muscles, especially after childbirth.
What causes a pelvic floor disorder?
It’s not always easy to figure out why you’ve developed a pelvic floor disorder, but knowing common causes can help you get the right treatment. Dr. Grisales and Dr. Toprani say that both subtle and obvious symptoms of PFDs are caused by:
- Obesity. Heaviness puts extra pressure on the pelvic floor muscles, which can weaken them over time.
- Muscle tightness or weakness in a more distant area that impacts your pelvic floor muscles.
- Chronic constipation. Straining to push out stool can weaken pelvic floor muscles. It might also be a sign that you have an overactive pelvic floor and those muscles can’t relax properly. (Click through to see how pelvic floor disorder can contribute to hemorrhoids.)
- Stress and habits, like chronic cough, hovering while peeing, or constantly trying to suck in your stomach. Stress can cause you to unconsciously clench your pelvic floor muscles. Sucking in and hovering above a toilet seat to pee can “confuse” the pelvic floor, make it hard for it to relax or contract when it needs to.
- Age and hormone changes with menopause that change the characteristics of your pelvic floor. Hormone fluctuations can lead not just to vaginal dryness, but tightening of the vaginal opening. Pelvic floor muscles also become thinner and less flexible.
- Pregnancy and childbirth. “A growing baby changes your posture and puts stress on your pelvic floor muscles,” Dr. Toprani says. “Pushing during vaginal delivery can tax them even more. And separation of abdominal muscles during pregnancy and cesarean delivery incisions can weaken the abdominal muscles that are connected to the pelvic floor.” Not fully healing after childbirth can lead to prolonged incontinence. “When a new mom is postpartum, rest often takes a backseat to newborn care,” Dr. Grisales says. “Your muscles are challenged by new activities like breastfeeding, bottle feeding, and holding your baby.”
Can I treat these issues at home?
Exercises and stretches may help improve your symptoms. Visit a pelvic floor specialist for a diagnosis, because some movements could worsen symptoms. (For example: If you have hypertonic pelvic floor muscles, or muscles that can’t relax, kegels may cause them to tighten even more.)
If you have a PFD caused by weakened pelvic floor muscles, physical therapy sessions and a doctor’s guidance are your best bet. If you have a PFD caused by a tight pelvic floor, relaxing exercises and stretches are an excellent way to supplement physical therapy. Dr. Grisales and Dr. Toprani suggest doing about 10 repetitions of these movements daily.
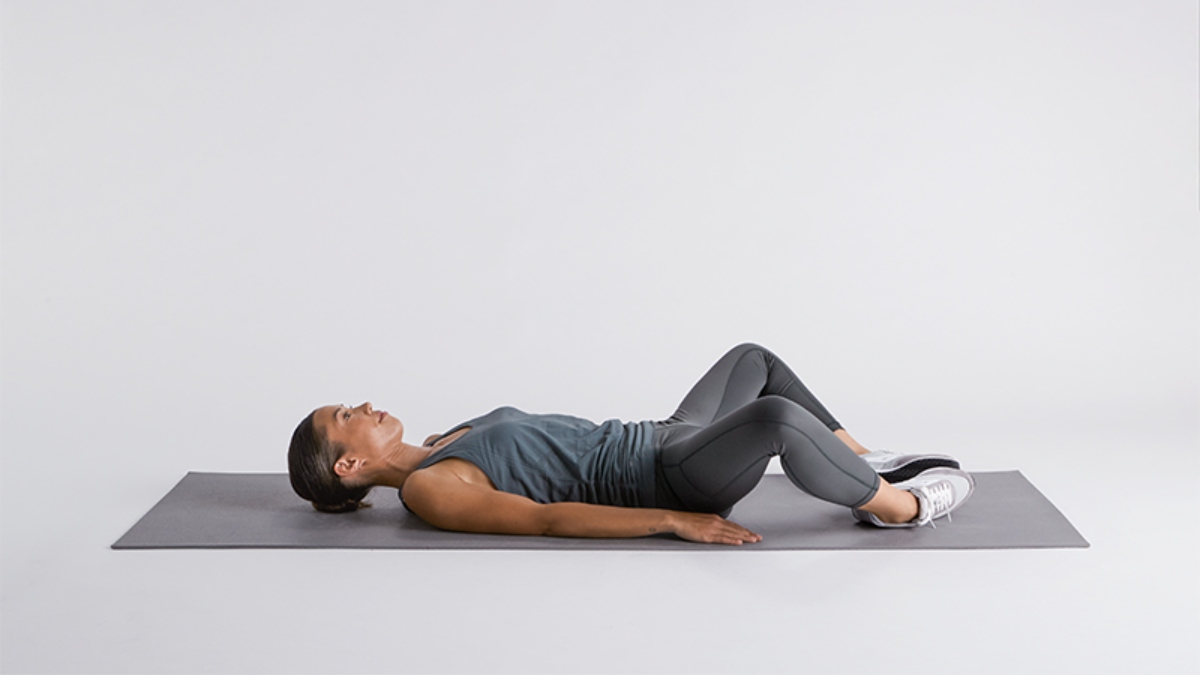
Diaphragmatic Breathing

“This is a form of deep breathing that helps relax and coordinate your entire core, including the pelvic floor to decrease pain and improve muscle function,” says Dr. Toprani. How to:
- Lie on your back with knees bent and feet flat on the floor.
- Rest one hand on your chest and the other on your belly.
- Slowly inhale through your nose as you fill your belly with air (so your hand on your belly rises up towards the ceiling). The hand on your chest remains mostly still.
- Focus on staying relaxed as you hold the breath in your belly.
- Slowly exhale through pursed lips, while the hand on your belly lowers with you.
Butterfly Stretch
“This stretch helps relax your inner thighs and pelvic floor muscles,” says Dr. Grisales. How to:
- Lie on your back with knees bent and your feet flat on the floor.
- Bring the soles of your feet together, and allow knees to fall comfortably toward your sides and to the floor. You should have made a big diamond shape with your pelvis, knees, and feet, and should feel a gentle stretch in your inner thighs.
- Direct your breath slowly towards your belly and pelvis as you hold this position.
- Slowly return to the starting position and repeat.
Note: If you have difficulty relaxing your abdominal muscles in this position, try doing the butterfly stretch sitting up.
Happy Baby

“This is a great exercise to open up your hips and help relax your pelvic floor muscles,” Dr. Toprani says. “A happy baby can help reduce pelvic pain, decrease the urge to urinate, and improve constipation.” How to:
- Lie on your back with knees bent and your feet flat on the floor.
- Draw knees up towards your chest, and reach your hands to grab the outside of your feet or ankles.
- While still holding your feet, slowly move your feet apart, stopping when you feel a gentle stretch in your inner thigh muscles and hips. Rock softly from side to side, if preferred.
- Breathe deeply and slowly. Relax back to the starting position and repeat.













