Goodbye, Bladder Leaks! Doctors Reveal the Best Urinary Incontinence Remedies
Turns out drinking *more* water lets you to laugh or sneeze without fear of an embarrassing leak

If you’ve ever laughed or sneezed only to realized that oops! you had a bladder leak, you know that urinary incontinence is no fun. And it’s more than just a hassle — loss of bladder control can be downright embarrassing. Fortunately, treatment for urinary incontinence doesn’t have to be hard or time-consuming. Keep reading for simple tricks you can try (often from the comfort of home) that help you sidestep leaks.
What is urinary incontinence?
Urinary incontinence is a condition characterized by the involuntary loss of urine, explains Jason Kim, MD, associate professor of urology and director of the Women’s Pelvic Health and Continence Center at Stony Brook University Medical Center. In other words, you can’t control when you urinate. Severity of urinary incontinence can range from occasional bladder leaks to the complete inability to hold urine in, Dr. Kim adds.
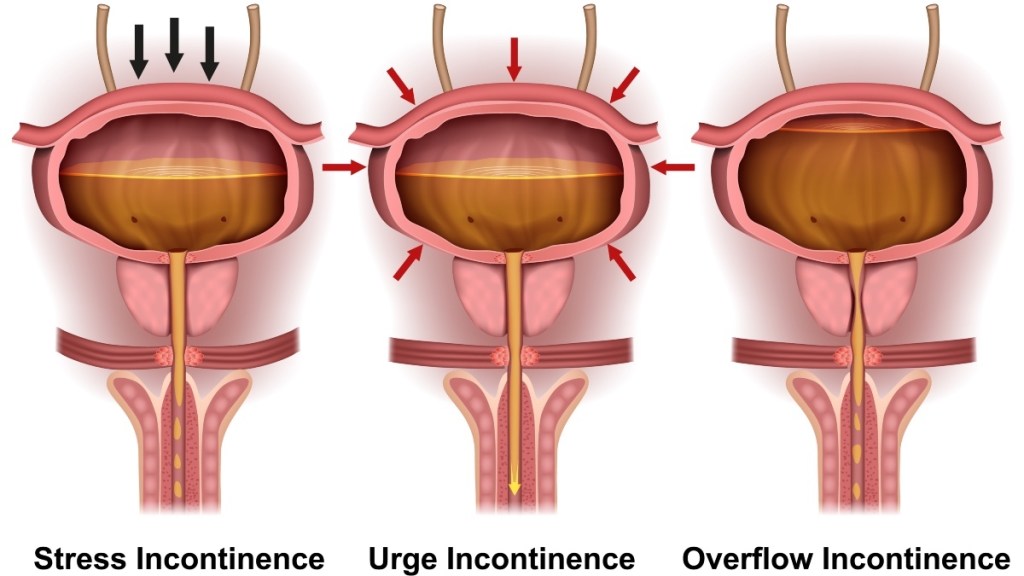
About one in three Americans are affected by urinary incontinence, and the condition affects twice as many women as men. There are four main types of urinary incontinence, according to Gil Weiss, MD, OB/GYN, assistant professor of clinical medicine in the Department of Obstetrics and Gynecology at Northwestern Memorial Hospital. They include:
1. Stress incontinence
This involves leakage during activities like laughing, coughing, sneezing or exercising. Pelvic muscle weakness is often at the root of this type of incontinence.
2. Urge incontinence
Also known as overactive bladder (OAB), this type of incontinence is a sudden and intense urge to urinate that can cause leaks. This can occur when the nerves that send signals between your bladder and brain aren’t working properly.
3. Mixed incontinence
This is the diagnosis you’ll receive if you experience both stress and urge incontinence.
4. Overflow Incontinence
Incomplete emptying of the bladder causes urine to build up and “spill out” involuntary when you have overflow incontinence. An overly distended bladder is often the source of the issue.
Common causes of urinary incontinence
“Urinary incontinence can have various causes, and often, multiple factors may contribute to the condition,” Dr. Kim says. He and Erica Montes, MD, board-certified gynecologist and pH-D Feminine Health advisor in Scottsdale, Arizona, say urinary incontinence can often be triggered by:
Pelvic muscle weakness
Weakened pelvic floor muscles due to aging, pregnancy, childbirth, obesity or even straining due to chronic constipation can lead to stress incontinence. What’s more, there is a natural loss of muscle tone and elasticity in pelvic tissues as women age. This can result in decreased support for the bladder and urethra, explains Mickey Karram, MD, a board-certified gynecologist, urogynecologist and obstetrician at Visthetic Surgery Institute and MedSpa in Beverly Hills, California. (Click through to learn the signs of a pelvic floor disorder and to learn how a pelvic floor massage can help.)
Menopause
Women over 50 are at a higher risk for urinary incontinence due to a combination of factors, “many of which are related to changes in the female reproductive and hormonal systems as well as the aging process,” Dr. Kim says. Reduced estrogen levels, especially during menopause, can contribute to weakening of the pelvic muscles and tissues.
In fact, 43% of women over 50 report experiencing urinary incontinence. And that number jumps to 51% for women age 65 to 80. “When the tissue by the bladder loses estrogen, it becomes thin, weaker and is more susceptible to bladder issues such as incontinence and urinary tract infections,” Dr. Montes adds. (Click through to learn how to thwart bladder spasms that trigger leaks.)
Diabetes
Diabetes can impair the nerves that control bladder function, triggering urges to go or making it hard to hold urine in. Other health conditions that affect the nerves, such as Parkinson’s and Alzheimer’s disease, can increase the odds of urinary incontinence, too. (Click through to find out how to reverse prediabetes and ward off bladder leaks in the process.)
Medications
Some over-the-counter and prescription medications, such as diuretics, antihypertensives and sedatives, may trigger urinary incontinence as a side effect. Click through to learn more about meds that cause bladder leakage.
The best treatment for urinary incontinence
“Consulting with a healthcare professional is crucial for an accurate diagnosis and appropriate management plan,” Dr. Kim says. “Some cases of incontinence may be temporary and reversible with appropriate treatment, while others may require long-term management strategies.” Here, the best natural treatment options for urinary incontinence.
1. Fill up with flaxseed
Fiber-rich foods like oats, beans and berries thwart constipation, a sneaky cause of bladder leaks. A study in Biomed Research International found that women who were constipated were more likely to experience moderate to severe overactive bladder symptoms. Researchers theorize this irritating effect may be due to a swollen colon pressing on the bladder.
To avoid this, aim to consume 25 to 30 grams of fiber a day, which helps keep your digestive system running smoothly to block backups. Also smart: Add 2 Tbs. of fiber-rich flaxseed to oatmeal or smoothies daily. The polyphenols in flaxseeds known as lignans have also been associated with nourishing the muscles that help hold urine in.
Tip: When possible, “avoid bladder irritants, like caffeine, alcohol, spicy, and acidic foods, to help prevent exacerbation of incontinence symptoms,” Dr. Karram advises.

2. Take a deep breath
A small study in Female Pelvic Medicine & Reconstructive Surgery found practicing daily mindfulness techniques helps relax a spasming bladder and reduces incontinence episodes. The good news: You don’t have to spend hours doing a complicated yoga meditation to get the benefits. Simply focusing on your breathing will do the trick! Try this: Choose one aspect of your breathing — air filling your lungs, for instance — and focus on that sensation for at least 30 seconds each day.
3. Give a squeeze
Research in JAMA Internal Medicine found that doing a 12-week pelvic floor muscle training program helped participants strengthen those muscles, which reduced incontinence episodes by 70%. An easy technique you can try at home? Kegel exercises. Simply tighten your pelvic floor muscles — the ones you’d use to stop urination mid-stream — for five seconds, relax five seconds, then repeat.
“Regular and correct performance of these exercises can improve muscle tone and provide better support to the bladder and urethra,” Dr. Kim says. You don’t need to be kegel-cizing all day long, but for best results, “repeat this process several times throughout the day.” Check out the video below for a quick visual how-to.
4. Stretch your legs
For added benefits in addition to kegels, spend 10 minutes practicing relaxed yoga poses and stretches daily. And focus especially on moves that tone the inner thighs, hips and glutes. A study in the Journal of Manipulative and Physiological Therapeutics suggests that strengthening hip muscles in conjunction with pelvic floor muscles improves bladder control. Any exercises that strengthen the core and support the pelvic region, such as yoga and Pilates, can be particularly beneficial, Dr. Kim adds.
5. Drink up
It may seem counterintuitive to drink more if you’re experiencing bladder leaks. But “staying adequately hydrated is important for overall bladder health, as dehydration can lead to concentrated urine and irritation,” Dr. Karram says. When urine is ultra concentrated, it’s rich in minerals that can irritate the bladder and make incontinence even worse. Dehydration can also increase risk for constipation.
So what does “adequate hydration” look like? The National Academy of Medicine has set 91 ounces as a daily goal for women, which you should spread out throughout the day. You can hit that goal via drinks (such as water, decaf tea and juice) and hydrating foods (like melon, berries, cucumber, leafy greens, grapes and celery). If your urine looks pale yellow or almost clear instead of golden or dark yellow, you’re probably near that target. (Click through to learn how a motivational water bottle can help you drink more H2O.)

6. Go when you’ve gotta go
Rather than waiting until the last second to sprint to the toilet, “make an effort to empty the bladder regularly and completely to help prevent over-distension and stress on the bladder,” Dr. Kim recommends. The “normal” number of times to urinate per day varies by person, but most people feel the need to go about every 3 to 4 hours, or 6 to 8 times per day. Your sweet spot may range from 4 to 10 bathroom visits per day, though.
Tip: When you do take a bathroom break, try a Mayo Clinic technique known as double voiding. The simple trick helps you fully empty your bladder. After urinating, lean forward as if you’re taking a seated back, then sit back upright and try to go again. This helps compress your bladder and squeeze out as much urine as possible, warding off leaks.
Advanced treatment options for urinary incontinence
If natural remedies aren’t providing enough relief for urinary incontinence, your doctor can help with more intensive treatment options. These include:
Treatment for urinary incontinence: Medication
For women whose urinary incontinence is related to menopausal hormonal shifts, Dr. Montes is a fan of vaginal estrogen treatment. This is a hormone cream that you apply directly to your vagina. “It’s excellent treatment for prevention and therapy,” she says. “It’s also safe, low-risk and can help reduce so many urinary symptoms, including recurrent urinary infections, overactive bladder and stress incontinence.”
Other pharmacological options (such as oral medications) work by relaxing the bladder, increasing its capacity or promoting the tone of sphincters that control urination.
Treatment for urinary incontinence: Surgery
Don’t lose hope if “conservative measures — lifestyle changes, pelvic floor exercises and medications — have not provided sufficient relief,” Dr. Karram says. Instead, see a urologist or urogynecologist.
“It’s not uncommon for specialists such as myself to see patients with urgency incontinence who have taken medications for over 20 years with no discernible improvement,” Dr. Kim says. “They usually have been told that there are no other treatment options available.”
But that’s not the case. There are several treatment options, including minor in-office procedures, that can provide dramatic relief. They include:
- A bladder botox injection. Ideal for patients with urge, stress, or mixed incontinence, a doctor injects botox into the bladder to send a message to the muscles to relax. This allows women more time to make it to the bathroom when they feel the need to urinate.
- Periurethral bulking. A doctor injects a bulking medium like collagen or a gel in and around the walls of your urethra, where urine passes. This is a frequent treatment for those with stress incontinence.
- Sling placement. A doctor uses either tissue transferred from another area of your body or a synthetic mesh sling to help support the neck of the bladder and the urethra during this minor surgical procedure. It’s often recommended as a treatment for stress incontinence.
- Percutaneous tibial nerve stimulation. To help treat urge incontinence, the American Urological Association (AUA) gives the green light to this tongue twister of a treatment. A doctor places an acupuncture-like needle near the ankle, which is attached to a nerve-stimulation device. It uses electrical pulses to retrain bladder nerves.
- Sacral neuromodulation. During this minor surgical procedure, a doctor inserts a bladder “pacemaker” of sorts. This helps the brain, bladder, and nerves work together more smoothly. The AUA suggests this for individuals with urge incontinence.
The bottom line: “Please know that urinary incontinence is common, but not necessarily normal,” Dr. Montes says. “If you have symptoms, please bring it up to your physician. If they say it’s not a big deal, ask for a referral. You don’t have to live with these symptoms.”
For more ways to outsmart bladder bothers:
Doctors Break the Silence on the Bladder Problem That Feels Like a UTI That Never Goes Away
Doctors Weigh In on The Best Natural Solutions for Female Bladder Problems
Top MDs: Common Prescription Medications Cause Bladder Leakage — How to Get Relief
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.












