Shiny Skin on Legs Could Be the First Sign of Peripheral Artery Disease — What Doctors Want You to Know
Women are more likely to have fewer symptoms, which can lead to underdiagnosis of the condition

It’s no secret that as we get older, our bodies start to react differently to the same activities. Clutching the pages of a paperback can cause cramping in the hands. Retrieving groceries from shopping bags can trigger back pain. And strolling around the neighborhood can lead to achy legs. But if that pain is confined to the calves and accompanied by shiny skin on the legs or uncomfortable maladies in the feet, it may be a clue that you have peripheral artery disease (PAD). Here, discover common (and sneaky!) peripheral artery disease symptoms, find out how to get tested, and see the MD-backed home treatments that ease discomfort.
What is peripheral artery disease?
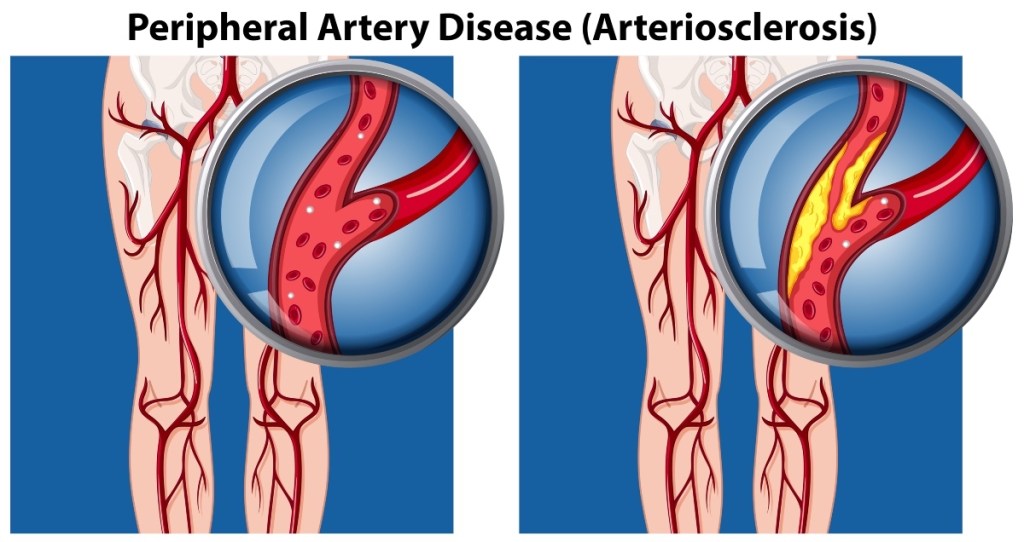
“Peripheral arterial disease is the development of atherosclerotic disease in the arteries of the legs,” explains vascular surgeon and PAD expert Britt Tonnessen, MD, an Associate Professor of Surgery (Vascular) at the Yale School of Medicine. “Over time, fatty deposits occur in the blood vessels and can progress to more complex areas of stenosis, or blockages.” You’ve likely heard of atherosclerosis, which is the fancy name for when plaque builds up in the arteries and eventually restricts blood flow. When this build-up occurs in the legs, it is referred to as peripheral artery disease.
“In peripheral artery disease, the legs or arms — usually the legs — don’t receive enough blood flow to keep up with demand,” adds cardiologist Evelina Grayver, MD, the Director of the Women’s Heart Program at the Katz Institute for Women’s Health in Queens, NY and an Assistant Professor in the Department of Cardiology at the Donald and Barbara Zucker School of Medicine at Hofstra University/Northwell. “This may cause leg pain when walking and other symptoms.”
People at risk for PAD
“The incidence of PAD increases with age, especially over 65,” says Dr. Tonnessen. “It afflicts 12% of the US population over the age of 40.” The prevalence of PAD is very low in women in their 40s (just 1.7% of women have the disease), but doubles in women in their 50s and jumps up to 25% of women over 80. Other risk factors include:
- Diabetes
- Obesity
- Smoking
- High cholesterol
- High blood pressure
- A family history of PAD, heart disease or stroke
- High levels of the amino acid homocysteine, which can increase the risk for coronary artery disease
Symptoms of peripheral artery disease
There are a few common symptoms of peripheral artery disease that can tip you off to the condition. The biggest one is claudication, or pain in the legs when walking. “Claudication is pain in the calf muscle with walking that is reproducible at a set distance,” explains Dr. Tonnessen. “For example, a person walks to her mailbox every day and the leg hurts by the time she gets there. The pain is relieved by standing or resting.” Other typical symptoms, according to our experts, include:
- Burning pain in the feet
- Coldness in the feet or in one foot but not the other
- Sores on the feet that fail to heal
- Your toenails and leg hair stop growing
- A pale or bluish color to the skin
While the symptoms above are some of the most common, there’s a PAD sign that can sometimes fly under the radar: shiny skin on your legs. This is what’s known as a trophic change. When oxygen- and nutrient-rich blood flow to your legs is diminished, it can make the skin on your legs appear shiny and pale rather than supple with a healthy flush.
Despite the fact that PAD is inherently a blood flow issue in the legs, Dr. Tonnessen cautions against confusing it with varicose veins. “Problems with the leg arteries are a bigger health risk and can be more difficult to diagnose,” she says. “Patients with PAD typically have no outward changes in the appearance of their legs, but may have pain in the legs and feet. Pain is your body’s warning sign.” (If you do have varicose veins, click through to learn how witch hazel for varicose veins can help.)

Related: Doctors Reveal the Best Sleeping Position to Outsmart Nighttime PAD Leg Pain
How peripheral artery disease symptoms affect women
While PAD is seen equally in both women and men, it can be more difficult to diagnose in women. “Women are more likely to have asymptomatic (silent) peripheral artery disease or to present with atypical symptoms, which can lead to underdiagnosis,” Dr. Tonnessen says. “Only about 50% of those with PAD have pain in their legs.”
There are also some conditions, according to the National Heart, Lung, and Blood Institute, that can be mistaken for or confused with PAD. This includes arthritis, vein problems, or nerve issues like sciatica. (Click through to learn how pseudo sciatica can mimic this pain, too — and find out how to treat it.)
“Symptoms of pain, aches, or cramps with walking claudication can happen in the buttock, hip, thigh, or calf,” adds Dr. Grayver. “So PAD often goes undiagnosed by healthcare professionals.” If the disease is suspected, a doctor will use your health and family history, as well as any symptoms, to decide whether or not to test for peripheral artery disease.
How PAD is diagnosed
Once your doctor determines that a test is necessary, it is relatively simple to diagnose PAD, notes Dr. Tonnessen. “An examination of the legs and feet will check for pulses,” she says. “Then the best screening test for PAD is an ankle-brachial index study. This is a test which uses blood pressure cuffs to compare pressure in the legs to the arms. Normal readings are >0.9 (essentially, 90% circulation in the lower legs). The lower the reading, the more serious the PAD.”
Lower readings may warrant additional tests. “Your doctor may also do imaging tests such as ultrasound, magnetic resonance angiography (MRA), and computed tomographic (CT) angiography,” says Dr. Grayver. She adds that while rare, the most serious cases of PAD can lead to gangrene or amputation. These tests can determine how quickly you need to act to reverse symptoms.
4 ways to ease peripheral artery disease symptoms
Sounds obvious, but a healthy lifestyle is the most effective strategy for treating PAD and its symptoms, says Dr. Grayver. The good news: It doesn’t have to be a chore! These smart tips ease pain and keep peripheral artery disease symptoms in check.
1. Take a daily aspirin
“I recommend my patients to take aspirin or other similar antiplatelet medicines to prevent serious complications from PAD and associated atherosclerosis,” says Dr. Grayver. According to the American College of Cardiology (ACC), both aspirin and clopidogrel (another antiplatelet medication) are recommended to reduce the risk of cardiovascular events or stroke in patients with PAD. Your doctor can determine the best daily dosage for you, but the ACC reports taking 75 mg. to 325 mg. of aspirin is a safe and effective PAD treatment.
2. Try the “red light, green light” trick
“The Society for Vascular Surgery and many other medical societies endorse walking as a way to improve vascular health,” says Dr. Tonnessen. “There is good evidence that walking can train the leg muscles in patients with PAD.” Engaging in a walking program can help folks build up to walking farther and longer without pain. The trick: Turn it into your own personal game of red light, green light. Walk until you feel pain, then stop for a break. When the ache subsides, resume your stroll.
“Walking regularly 20 to 30 minutes a day at least 5 days a week is what I advise,” Dr. Tonnessen adds. “For those who can only walk short distances due to the claudication, include the rest times in the total walk times. Stop, stand, and then go again when the pain improves. Over a period of six to eight weeks, a person with PAD may be about to double her walking distance.”
The proof: A review in the Journal of Cardiopulmonary Rehabilitation and Prevention found that regular walking (whether strolling outside or on a treadmill) help PAD patients walk up to 420 ft. farther pain-free within 12 weeks. And a separate study in the Journal of Vascular Surgery found that when folks with claudication walked as little as two to three times per week until they felt pain (then stopped before resuming), there were able to walk more than twice as far. What’s more, their blood vessels were up to 82% more dilated within 12 weeks, a sign of improved blood flow. (Ready to start stepping? Click through for a round up of our favorite ultra-comfortable Jambu walking shoes.)

3. Eat like an Italian
Enjoying more low-fat (or healthy fat) foods is a smart strategy for improving your cardiovascular health, says Dr. Grayver. Whenever possible, replace foods like butter, fatty cuts of meat, and high-fat cheeses with healthier fare such as olive oil, fish and grains and beans. Better yet, consider adopting a Mediterranean diet. (Click through for a tasty Mediterranean diet meal plan.)
A review in Circulation Research that looked at 45 studies confirmed that the evidence in favor of a Mediterranean diet for cardiovascular health is “large, strong, and consistent” and is associated with better cardiovascular health outcomes. That translates to a reduce risk of coronary heart disease, ischemic stroke, and total cardiovascular disease, all of which can worsen peripheral artery disease symptoms.

4. Opt for “hot-cold” therapy
A spa-inspired way to boost blood flow and alleviate peripheral artery disease symptoms: Indulging in heat and cold therapy. “A more ‘out of the box’ treatment may include sauna treatments followed by cold plunges, allowing for more blood flow to develop,” says Dr. Grayver. A study in Physical Therapy confirms that the combination of hot and cold treatment improves mean blood velocity, or the speed at which blood is able to travel through the arteries. No access to a sauna? No problem! You can achieve the same benefits in the shower using hot and cold water. The researchers found that the optimal ratio is three minutes of heat followed by one minute of cold.
For more ways to treat common vascular conditions:
The 8 Best Natural Remedies For Varicose Veins According To Vascular Specialists
Tired, Achy Legs? Here Are 4 Tips to Ease Peripheral Artery Disease Symptoms
Natural Ways To Erase Broken Blood Vessels On Your Face — Quickly and Permanently
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.