Ob/Gyn: 1 in 5 New Cases of Cervical Cancer Are in Women Over 65 — Here’s What You Need to Know About HPV in Seniors
The strains of the HPV virus that lead to cancer can lay dormant for years so don't stop getting your PAPs!
Those of us over a certain age likely don’t spend much time thinking about the human papilloma virus (HPV). Despite the fact that the sexually transmitted virus is estimated to infect 4 out of every 5 women by the time we turn 50, we tend to think of HPV as a worry for the younger crowd — people in their 20s and 30s, not seniors. But do older adults, especially those in long-term, committed relationships need to be concerned? We asked two top MDs to weigh in on everything you need to know about the country’s most common STI, including how often you should get screened and why an abnormal PAP smear shouldn’t automatically be a cause for worry.
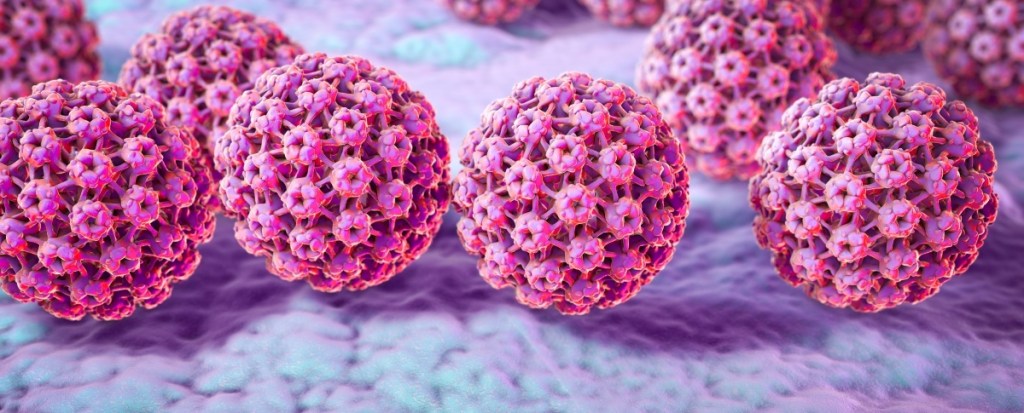
HPV can lie dormant, then reactivate in seniors
HPV is a sexually transmitted infection spread through intercourse with someone who has the virus. The infection can spread even though a person isn’t showing signs or symptoms of an active infection. And for those who do contract HPV, you may not show signs for years.
Risk of contracting HPV may be highest when you’re young, but unfortunately, that doesn’t mean older women (and men) are out of the woods, says ob/gyn Barbara DePree, MD, a certified menopause practitioner and founder of MiddlesexMD.com, an educational resource for women’s sexual health in perimenopause and beyond.
“HPV can lie dormant in the body for years, only to become an active infection as the aging immune system grows too weak to suppress it,” she says. In fact, she notes that HPV is the most common cause of “abnormal” Pap smears. What’s more, a study in the Journal of Infectious Disease found that a latent HPV virus more likely to activate at onset of menopause. Dr. DePree likens this HPV reactivation to getting chicken pox as a child, then contracting shingles years down the road.
Indeed, in a study of 1,550 women between the ages of 57 and 85, 1 in 16 had a high-risk strain of HPV (i.e., one of two strains that can lead to cancer) — and this was not correlated with how sexually active they were.
Why so many seniors are unaware they have HPV
“We have a large population, that includes women over the age of 65, who have HPV,” says Chicago ob/gyn Lauren Streicher, MD, Clinical Professor of Obstetrics and Gynecology at Northwestern University’s medical school, The Feinberg School of Medicine, and host of Dr. Streicher’s Inside Information: Menopause, Midlife and More Podcast. She adds many don’t even know they have it. Why? Doctors only started using the HPV test (which was developed in 1999) as a screening tool in the last 20 years, she says. “Not only does the virus come and go, but Pap smears 20 years ago didn’t test for HPV.” At the time, she says, experts believed that cervical cancer was caused by the herpes virus, so HPV tests weren’t a priority.
What’s more, an HPV test only detects an active infection, Dr. Streicher says. That means a woman who’s told she doesn’t have HPV based on her most recent screening could still harbor a dormant virus. Likewise, a woman who’s told for the first time that she has HPV (say at age 50 or 55) could have had it for decades. “If you have HPV that was just detected today, there is no way to tell when you acquired it, even you’ve had negative HPV tests in the past,” Dr. Streicher notes. “It could have been three months ago or 30 years ago.” This is why doctors still screen for HPV even among patients who’ve had no new exposure to the virus.
The most common signs and symptoms of HPV
Although Dr. DePree says most strains of HPV are harmless and cause no symptoms, some can trigger warts. Some appear as raised patches on the skin and others can look like cauliflower, with bumps and stem-like protrusions. Often they are genital warts that appear on the vulva, cervix, vagina or near the anus.
“Genital warts are unpleasant to deal with because they can be itchy and uncomfortable,” Dr. Streicher says. “Sometimes they go away on their own. But we can also treat them and there are a number of ways to do it.” Some of the more common treatments are medication and topical creams. Your doctor may also recommend dissolving the wart with an acid. “We can also remove them surgically, but they can recur.” (Not sure if you have genital warts or vaginal boils? Click through to learn how to tell if you have a vaginal boil — and how to treat it.)

Complications of an HPV infection
While most types of HPV aren’t problematic, some high-risk types — specifically types known as 16 and 18 — can lead to cancer. This includes cervical, vulvar, vaginal, penile and anal cancers, as well as cancers of the head and neck. (Click through to our sister publication to learn how to prevent cervical cancer.)
“A persistent HPV infection that doesn’t clear can develop into pre-cancer or cancer,” says Dr. Streicher. “But this happens very slowly. For people who do get cancer, it doesn’t happen for years, which is why screening is so important.” Once you (and your doctor) know that you have HPV, regular screenings will pick up any changes that can indicate cancer early enough to keep you safe, she says. “If someone is told they have HPV it doesn’t mean they’re going to get cancer. In fact, the overwhelming number of people don’t. It just means they’ve been exposed and should be monitored to make sure it doesn’t cause problems down the road.”
How often seniors should get screened for HPV
For years, an annual exam and Pap smear were recommended. But because the HPV-driven changes to cervical cells that can lead to cancer happen very slowly over time, those guidelines were changed. The United States Preventative Services Task Force (USPSTF) currently advises a Pap test every three years for women ages 21 to 65, or a Pap test plus HPV test every five years for women ages 30 to 65. Additionally, the guidelines suggest that women who are older than 65 who have had “adequate screening” and are at low risk for cervical cancer no longer need to be screened.
“There is a lot of concern over this, because what we’re starting to see now is that one in five new cases of cervical cancer are in women 65 and older. And 70% are being diagnosed at a late stage when it’s less treatable,” Dr. Streicher says. She says many women assume that if they don’t need Pap or HPV tests, they can also forgo their annual check-ups. “The majority of women over age 65 are not seeing their gynecologists. Not only are they not getting a Pap test, but they’re getting no visual inspection.”
Dr. Streicher recommends that all women over the age of 50 get an annual gynecological exam. “The frequency of Pap tests depends on their personal and medical history,” which can be discussed when you see your doctor, she adds.

Risk factors for HPV in seniors
Reactivation of the virus is a likely reason for seniors to be diagnosed with active HPV. But new infections can also occur. “Just because you’re 65 doesn’t mean you stop having sex,” notes Dr. Streicher. “People get divorced, spouses die and people get remarried.” But older folks with new sexual partners are less likely to use protection. “Pregnancy is no longer an issue. But an older woman is more vulnerable to HPV because her tissue is thin and more likely to tear.” What’s more, a study in the Journal of Infectious Disease found incidence of HPV is higher in men than in women. That’s why Dr. Streicher advises all of her patients who begin new relationships use condoms.
But new sexual partners aren’t the only risk factor for HPV. “People who smoke are less able to clear an HPV infection,” Dr. Streicher says. Scientists suspect that DNA damage caused by smoking impairs the immune system’s ability to fight off HPV. “Smoking affects cells throughout the body and is associated with so many diseases and different types of cancer.”
Stress may also play a role, she says. In fact, researchers reporting in the journal BMC Cancer found that chronic stress and large changes in levels of the stress hormone cortisol from morning to night may play a role in HPV-induced cervical cancer. (If you’re often anxious and exhausted, it might be mitochondrial dysfunction.)
More ways to ward off cancer caused by HPV
To help lower your risk of cervical cancer, eat a variety of fruits and vegetables every day, suggests Dr. DePree. These foods contain nutrients such as antioxidants, carotenoids, flavonoids and folate. These help the body fight off HPV and prevent an HPV infection from turning healthy cervical cells into cancerous ones.
And Dr. Streicher suggests getting the HPV vaccine. “The FDA has approved the HPV vaccine up until age 45,” she says. “The immunological response to the vaccine is not going to be as robust after that. But it will still offer some protection and there are no safety issues. Plus, there is some data that shows the vaccine does help clear an HPV virus you already have. I think it’s appropriate for women to discuss with their physicians.”
Not in the mood as often lately? Read on to discover how to boost your libido naturally:
- Expert Advice: ‘My Sex Drive Dropped. Is There a Natural Option Instead of HRT?’
- Can Acupuncture Boost Your Sex Drive? Here’s What An Expert Has To Say
- If Menopause Put Your Sex Drive on Pause, Here’s How To Get It Back… Naturally
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.