MDs Reveal the Home Cures That Soothe Hemorrhoid Itch & Discomfort In Minutes
Plus, the right way to wipe so you don't make it worse!

If you’ve ever had a hemorrhoid flare-up, you know that it can be hard to think of anything other than the intense discomfort that comes with it. One of the most common symptoms of hemorrhoids, along with irritation, bleeding, and soreness is itching. And while the itching is uncomfortable during the day, it can feel even more intense at night. Here, top experts weigh in on why hemorrhoids itch at night — and the simple home cures that work even better than some over-the-counter creams.
What are hemorrhoids?
“Hemorrhoids are a natural part of our body,” says Lynn M. O’Connor, MD, a colorectal surgeon and chief of colorectal surgery at both Mercy Hospital and St. Joseph Hospital in New York. “They’re vascular cushions in our anus and everyone has them.” These anal cushions, aka hemorrhoids or piles, are made up of connective tissue, blood vessels, and a small amount of muscle. Hemorrhoids actually serve an important purpose by helping to shield the skin around the anus from passing stool.
“Normal hemorrhoidal tissue is there to maintain continence. It keeps the rectum closed so that stool doesn’t leak out,” explains gastroenterologist Eric Dinesh Shah, MD, a clinical associate professor of medicine at the University of Michigan in Ann Arbor and a spokesperson for the American Gastroenterological Association.
But problems occur when excess pressure is put on these cushions. This can make the veins and blood vessels in your lower rectum or around your anus painfully swollen and inflamed — what most of us consider “hemorrhoids”. It’s not uncommon. According to the National Institute of Diabetes and Digestive and Kidney Diseases, hemorrhoid flares affect 1 in 20 Americans. And the the issue worsens with age, impacting about half of people over 50.
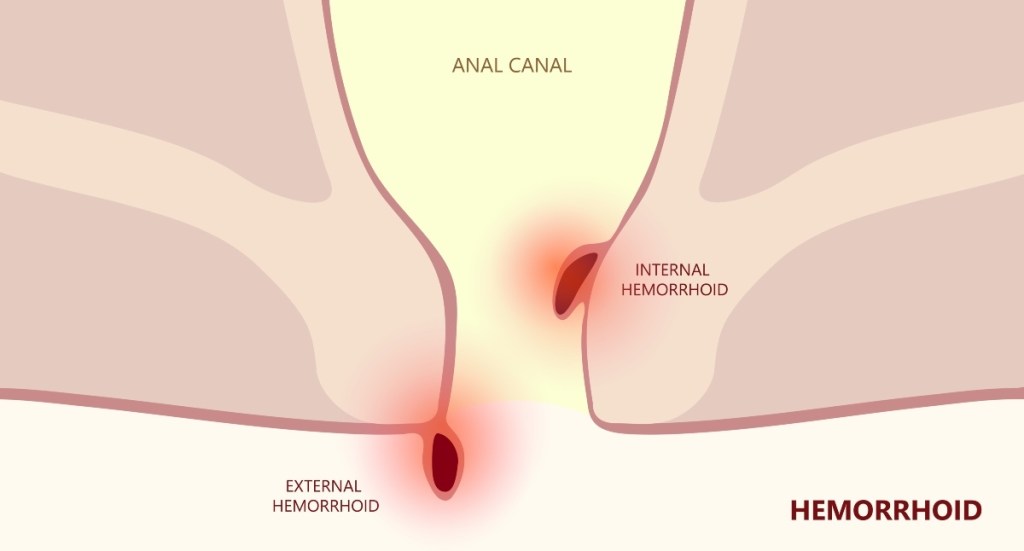
The two main types of hemorrhoids
There are two types of hemorrhoids: internal, which form in the lining of your anus and lower rectum, and external, which form under the skin around the anus. External hemorrhoids are the more uncomfortable of the two because they’re outside of the anus. There, they can rub against clothing or play host to mucus or stool particles, which can cause irritation and itching.
Internal hemorrhoids tend to be painless, though they can bleed. You’ll likely notice blood on toilet paper or in the toilet after using the bathroom. But if you see blood after wiping or in your stool for a prolonged period of time, it’s time to schedule a visit with your doctor. “With bleeding we can’t always assume it’s hemorrhoids,” Dr. Shah says. “It could be sign of something else, such as inflammatory bowel disease, ulcers, or possibly a sign of cancer. It can be hard to tell without an evaluation, including a colonoscopy, to take a look as to what’s really going on.”
What causes hemorrhoids?
Some of the more common causes of hemorrhoid flare ups include overexerting yourself when having a bowel movement (such as passing too-hard stool or straining due to constipation), lifting heavy things, prolonged sitting (especially on the toilet), pregnancy and being overweight. This puts pressure on your hemorrhoidal tissue, weakening and stretching the veins there.
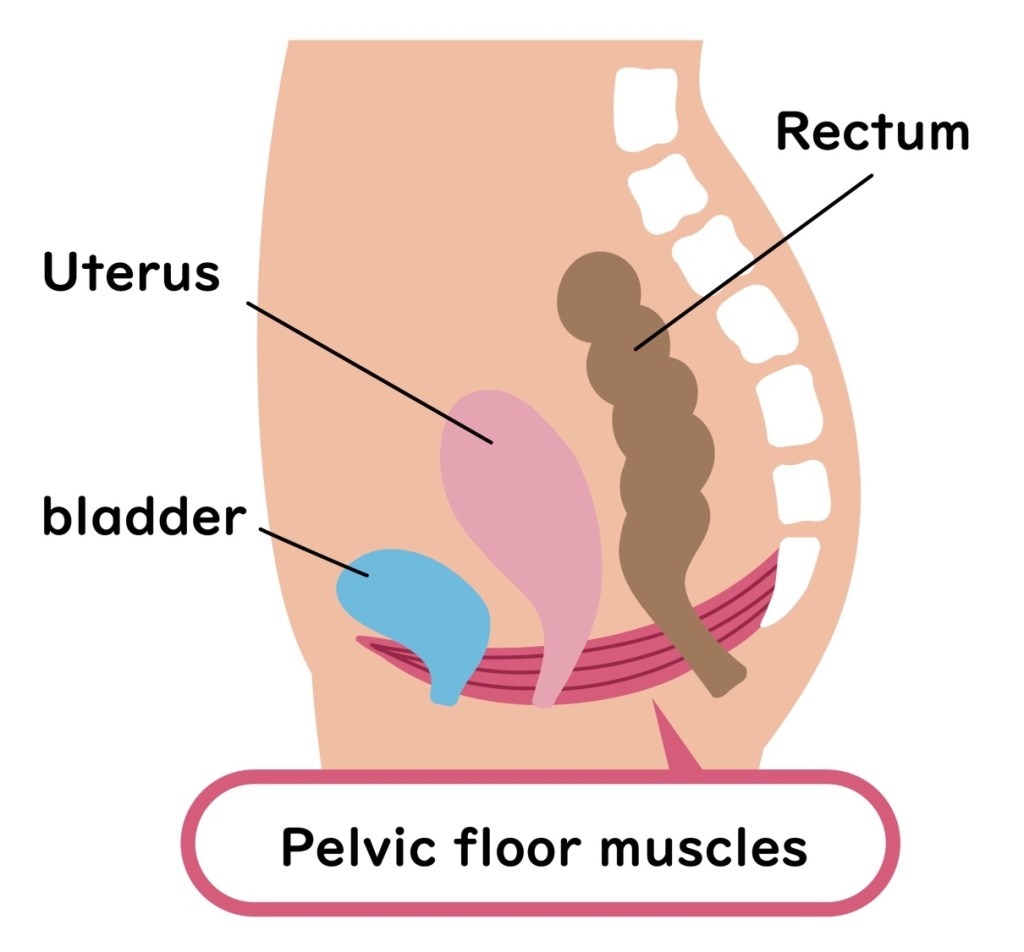
An under-the-radar trigger? Pelvic floor dysfunction, says Dr. Shah. Your pelvic floor consists of the muscles and the connective tissue that support organs in your pelvis including your bladder, bowel, and reproductive organs. “Pelvic floor dysfunction is caused by poor coordination or weakness of the pelvic floor when straining, which in turn is a common cause of hemorrhoids,” he explains. The condition affects approximately 25% of women in the US. (Click through to see the telltale signs a pelvic floor problem,)
Who is most at risk for hemorrhoids?
More people over 50 experience hemorrhoids because as we age, the connective tissue between the anus and rectum gets weaker, explains Dr. Shah. “Increased pressure, especially if you’re straining to have a bowel movement, can make it easier for an external hemorrhoid to break through.”
What’s more, “older adults are more likely to experience constipation from lack of adequate physical activity, a low-fiber diet or taking certain medications, such as those for high blood pressure and depression,” Dr. Shah explains.
You may also have your family to thank for your hemorrhoids. When researchers reporting in the journal Gut examined cells of nearly one million people, they identified genes in 102 regions of the human genome that increase the risk of hemorrhoids. And the American Academy of Family Physicians says people whose parents had hemorrhoids may be more likely to have the painful, itchy condition, too.
Why do hemorrhoids itch at night?
Let’s start with why hemorrhoids itch in the first place. “If hemorrhoids are inflamed, that can cause itchiness,” says Dr. O’Connor. “You also can experience itchiness from the friction of the toilet paper if you’re wiping excessively. And if hemorrhoids are swollen and hang down, they can rub against clothing.”
When it comes to nighttime itchiness, Dr. O’Connor says one reason it may feel worse is because you’re more fixated on it. “You might be more aware because there’s nothing to distract you from the itching,” she says. “During the day, you’re doing what you need to do and dealing with other things so you might not have time to focus on it that much.”
And while you’re sleeping, you may be unaware you’re scratching the area. That’s a problem, since scratching inflamed hemorrhoids can potentially make the problem worse. “Scratching can cause an itching and scratching cycle that doesn’t stop,” says Dr. Shah, increasing inflammation.
The best ways to soothe hemorrhoid itching
Whether itching and irritation strikes at night or flares up during the day, these simple, natural home remedies can quickly quell symptoms.
Dab on witch hazel
When symptoms flare, pat the problem area with a cotton ball dampened with witch hazel. This natural astringent has been a folk cure for hundreds of years to relieve itching, and research now proves it really is one of the best ways to calm symptoms in seconds. That’s because witch hazel brims with tannic acid. And research in ACS Applied Materials and Interfaces found this compound shrinks swelling on contact and dulls inflamed nerve endings that telegraph pain. (Click through to our sister site to see 8 surprising uses for witch hazel and how witch hazel can shrink varicose veins) Need relief on the go? Reach for a pre-moistened, witch hazel-infused pad. One to try: Tucks Medicated Cooling Pads (Buy from Walmart.com, $7.68)

Relax with a warm sitz soak
A sitz bath, a shallow soak where water only covers your hips and bottom, can provide powerful relief from hemorrhoids. Research in the Women and Birth finds that taking a five-minute break three times a day to soak the affected area in warm, Epsom-infused water relieves pain and itching even better than topicals like Preparation H and Anusol. Not only does the warmth boost circulation to speed healing but the magnesium in Epsom salts also extinguishes pain-triggering inflammation. Tip: Try an Epsom salt blend formulated just for sitz baths. They’re dosed with anti-inflammatory ingredients like aloe, lavender and calendula. One to try: Lansinoh Sitz Bath Salts (Buy from Amazon.com, $12.03)
Tip: When washing and drying the anal area, be extra gentle. “Skin can break down if you’re washing too aggressively,” cautions Dr. O’Connor, which can worsen irritation. You also want to pat the area dry with a soft cloth instead of rubbing in a “flossing” motion. Or you can use a hair dryer on a low cool or warm setting, Dr. O’Connor adds.
Try a citrus plant extract
Taking a potent citrus plant flavonoid called diosmin daily slashes hemorrhoid symptoms up to 67%, according to a review of 10 studies in the British Journal of Surgery. What’s more, it cuts your chances of a future flare up by 50% when taken daily. Diosimin improves blood flow, helping to constrict and heal the overly dilated blood vessels responsible for pain and swelling. Best of all, it begins working in as little as four days.
The best ways to ward off future flare-ups
After experiencing the pain and discomfort of a hemorrhoid flare, odds are you’ll want to do whatever you can to block a future one. Here, the best ways to curb your risk.
Sip a tropical smoothie
Starting each day with a frozen mango fruit smoothie blocks chronic constipation better than with the top MD-recommended treatments like psyllium fiber or laxatives, according to Texas A&M University. The reason? While fiber supplements and laxatives may aid in the treatment of constipation (the number-one underlying cause of hemorrhoids) they don’t fully address all the symptoms, such as intestinal inflammation.
But mangoes’ combination of soluble fiber and inflammation-fighting polyphenols heal the gut, preventing your system from backing up. Simply blend 1 cup fresh or frozen mango cubes with 1 ¼ cup plant or dairy milk. Enjoy! (Click through to our sister site to check out the genius hack for peeling a mango in seconds.)

Top your burger with creamy avocado
The American Society of Colon and Rectal Surgeons (ASCRS) recommends eating between 20 to 35 grams of fiber each day, with for reason: Shoring up fiber intake reduces hemorrhoid symptoms by 50%, suggests a study in The World Journal of Gastroenterology. Fiber helps create softer stools that pass more easily, which reduces the straining that triggers hemorrhoid pain. Some good options: topping your burger with sliced avocado or snacking on a handful of nuts daily.
Drink another glass of H2O
Another reason to chug more water: Adequate H2O blocks hemorrhoid-triggering constipation. Aim to drink about half your body weigh in ounces daily. “If you get 20 to 30 grams of fiber a day and drink plenty of water, you should be able to move your bowels with no problem,” notes Dr. O’Connor. (Click through to our sister site to check out the motivational water water bottle makes it easier to drink up.)
And if you do get that “gotta go” urge, don’t wait to make a trip to the bathroom. Delaying a bowel movement and holding in stool can cause the colon to absorb more water from the stool, making it drier and harder to pass.
Put your feet up when you go
Propping your feet up on a 7″ to 9″ footstool when you have a bowel movement cuts down on straining and toilet time (a top hemorrhoid trigger), a study from The Ohio State University found. When folks used a footstool for two weeks, 71% reported experiencing faster bowel movements and 90% reported less straining. Researchers say propping your feet up mimics a natural squatting position that relaxes the pelvic floor and makes it easier to “go”. Sitting on a toilet on the other hand, creates a bend in the rectum, which makes it more difficult to have complete bowel movement.
Read on for more ways to outsmart constipation, the top cause of hemorrhoid flares:
- Research: Castor Oil Packs Proven to Relieve Constipation, Menstrual Cramps & Joint Pain
- Having Trouble Going to the Bathroom? Try These 4 Natural Cures for Constipation
- A Doctor’s Advice: ‘How Can I Naturally Ease Constipation — Without Prunes?’
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.
A version of this article originally appeared in our print magazine, Woman’s World.